Summary on Webtool to Enhance the Accuracy of Diagnostic Algorithms for heart failure with preserved ejection fraction (HFpEF)
Disclaimer before you continue: The content of this page is generated to facilitate the interpretation of research to individuals interested in cardiovascular healthcare. The content is not intended for personal medical advice. Summaries and interpretations of the authors of a study do not reflect my professional opinion. Research often takes years to decades before results are developed enough to implement in clinical healthcare because new findings need to be extensively validated before we consider them safe enough for individual patients. Always consult your own professional healthcare provider for medical advice.
Klik hier voor Nederlandse samenvatting
The original article that is summarized on this page can be found here: https://doi.org/10.1002/EHF2.14525
#HFpEF diagnostic algorithms are applied more accurately with our webtool
Otherwise accuracy can be 🔻
This prospective study was possible thanks to collaboration and community participation! Many of 🫵you, thanks!
🗒️https://t.co/DAsKybX1zg #OpenAccess @escardio pic.twitter.com/RPftpNVsTT
— Jerremy Weerts, MD (@JerremyWeerts) September 19, 2023
Background information
Heart failure is a heart condition characterized by the inability of the heart to supply enough oxygen rich blood to body organs. Consequently, patients with heart failure experience symptoms such as shortness of breath during physical activities or fatigue. In the Netherlands roughly 240.000 individuals are diagnosed with heart failure. Half of these individuals have heart failure with preserved ejection fraction (HFpEF). Preserved ejection fraction means that the pump function of the left chamber of the heart is working normally. Rather, heart failure is present due to diastolic dysfunction and a stiffened left chamber of the heart, causing an inability to fill appropriately. Patients with HFpEF often have other cardiovascular diseases or risk factors such as hypertension, diabetes mellitus, atrial fibrillation, or impaired kidney function.
How to diagnose HFpEF?
Diagnosing HFpEF is challenging. Definitions of the syndrome have changed over the past years. Simply put, diagnosis requires signs and symptoms of heart failure, a preserved ejection fraction, and markers of heart failure in the blood or on ultrasound of the heart. Several recommendations have been given by international experts to better identify which relevant patient and heart-specific markers indicate HFpEF. The most recognized recommendations are the HFA-PEFF and H2FPEF algorithms, originating respectively from Europe and the United States. The results of following these algorithms provide a numerical score with a corresponding category. The category indicates the likelihood of a patient having HFpEF. The first category is ‘low’ and suggests HFpEF is unlikely the cause of symptoms. The second category is ‘intermediate’ and suggests HFpEF is possibly the cause of symptoms, but requires additional testing. The third category is ‘high’ and suggests HFpEF is probably the cause of symptoms.
Applying the HFA-PEFF or H2FPEF algorithm in clinical care is time-consuming and may be prone to errors. As a consequence, diagnostic errors may be made. This can result, for example, in too many additional tests for a patient to find out the correct diagnosis.
Methods used by the researchers
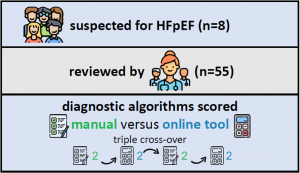
An online platform was created where 8 fictional patient cases suspected of having HFpEF were provided to participants. Participants were cardiology residents (in training to become a cardiologist), cardiologists, and cardiologists with heart failure expertise. Participants came from different countries worldwide. Their opinion was asked on every fictional patient case. Also, their use of the HFA-PEFF and H2FPEF algorithms was tested. In half of the cases, a webtool was provided to help the physician participants with scoring the algorithms.
Results of the study
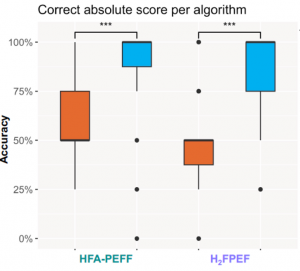
Fifty-five physician participants completed the study. They were mostly based in Europe. Participants had a correct result (score) of the HFA-PEFF and H2FPEF algorithms in only 50% of cases when no webtool was provided. This resulted in correct diagnosis likelihoods in 75%. Providing a webtool for the HFA-PEFF and H2FPEF algorithms improved the correct scores to 100%.
Using the HFA-PEFF and H2FPEF algorithms led to more agreement diagnostics between physicians. When correct scores were provided to participants, the diagnostic decision was changed in up to 2/3 of cases.
Discussion by researchers of the study
The researchers concluded that the current HFA-PEFF and H2FPEF algorithms are prone to errors. Providing tools to use these algorithms greatly improves the errors and can result in different diagnostic decisions by physicians. Because using a webtool still costs time, tools that better integrate with a hospital system and that do not require too much manual input are preferred for clinical use.
Reflection and open questions
My personal reflection on this study is biased because I have designed and conducted the study. Still, I think innovations that do not cost anything, can save time, and enhance the accuracy of clinical decisions are worth pursuing. The provided webtool, which is also available on my website (https://jerremyweerts.nl/tools/hfpef-calculator/) still demands a lot of manual input from physicians and would benefit from a more time-efficient design. We are working on that.
Even though this webtool provides more accurate algorithm results, it is unclear how much additional testing can be saved. Two important reasons. The first is that this study did not prove that physicians less often score an ‘intermediate’ likelihood for HFpEF, which prompts additional testing. The second is that additional testing is not only performed for HFpEF diagnosis. HFpEF is a syndrome that can have a variety of causing factors that require specific treatments, and additional testing is often needed to identify these factors.
The evolving insights into the HFpEF syndrome will likely prompt new diagnostic algorithms. The complexity of such algorithms will determine if webtools or digital tools will be useful.

Leave a Reply
Want to join the discussion?Feel free to contribute!